According to Dr Jean-Marc Dersot, plaque control is a crucial but often neglected factor in successful orthodontic treatment. Dr Dersot is a past president of the French Society of Periodontology and Oral Implantology, but his favourite topic remains the relationship between orthodontics and periodontics, and his output on the subject as a researcher is prolific. “In order to avoid side effects, orthodontists need to safeguard the periodontal tissue,” he stressed.
Dr Dersot, where do problems during orthodontic treatment usually arise?
For several decades, orthodontists and periodontists have claimed that orthodontic treatment holds no harmful consequences for a healthy periodontium. However, a systematic review of the literature undermined this common refrain and concluded that, even when periodontal conditions are optimal, slight adverse effects are to be observed. According to the overview, 12 studies, including 11 non-randomised ones, showed 0.03 mm gingival recession, 0.13 mm bone loss and 0.23 mm pocket depth at minimum. The conclusions of this meta-analysis are clear: there is no reliable evidence of the benefits of orthodontic treatment for periodontal health, and at best, mildly adverse effects are to be expected.
What should orthodontists do to avoid the worst problems?
In order to minimise the side effects of orthodontic treatment on the periodontium, orthodontists must be able to distinguish between patients they can immediately offer orthodontic treatment to and those who need periodontal treatment first. Before starting treatment, orthodontists should see their patients through the eyes of a periodontist.
Firstly, it should be a basic competence of all orthodontists to be able to recognise the eight signs of periodontitis: gingival bleeding, pain and sensitivity, abscesses and suppuration, gingival recession, tooth mobility, secondary migrations, food impaction and bad breath.
Secondly, orthodontists should know the six risk factors of periodontitis: a family history of periodontitis, a negative response to psychological stress, tobacco consumption, susceptibility to infections, partial or total cario-resistance, and a history of acute necrotising ulcerative gingivitis.
If any of these signs or risk factors are present, the orthodontist should send the patient to the periodontitis before any other treatment is undertaken in order to avoid further problems. Integrating periodontal concerns into orthodontics is essential, and having hygienists in orthodontic clinics is a huge help.
“A healthy periodontium is a prerequisite to beginning orthodontic treatment”

What about gingival recession?
The aetiology of gingival recession is multiple, but one cause is a given: lack of bone owing to dehiscence or fenestration. Several papers on modern dry skulls conclude that bone dehiscence and the resulting recessions are present physiologically.
A lack of bone can also become an issue during treatment. One of the current trends in orthodontics is that of no extractions, which also means that there are limits to the buccal movement of teeth. When a part of the root is outside the bone corridor—even if the gingivae are at a normal level—the orthodontist has created an at-risk site for gingival recession.
The great majority of recession happens at the anterior mandibular teeth, and in the symphysial area, the bone is very thin. So I can imagine that it is sometimes difficult to perfectly control the angulation of anterior mandibular teeth and the position of the roots in the bone corridor.

So where does plaque control come in?
A healthy periodontium is a prerequisite to beginning orthodontic treatment. It is mainly because of periodontal tissue and, more particularly, the periodontal ligament that the orthodontist is able to move teeth. However, gingival inflammation with a high hyperplasia compound, periodontal attachment loss, bone loss and root resorption can cause a reduction in periodontal support. The key to preventing these problems and minimising side effects is plaque control. The objective of plaque control is to avoid or stabilise gingival inflammation after periodontal treatment and to avoid or minimise the deleterious side effects of orthodontics on the periodontium.
The challenge before orthodontic treatment, both in children and adults, is to change patient behaviour when it comes to plaque management and instil good brushing habits. Inflammation due to dental plaque leads to gingival recession if a bone dehiscence is present. Also, a heavy brushing technique can create micro-wounds which can cause recession. For these reasons, efficient, atraumatic plaque control is a key factor in successful orthodontics.

What kind of brush should dental professionals recommend to patients?
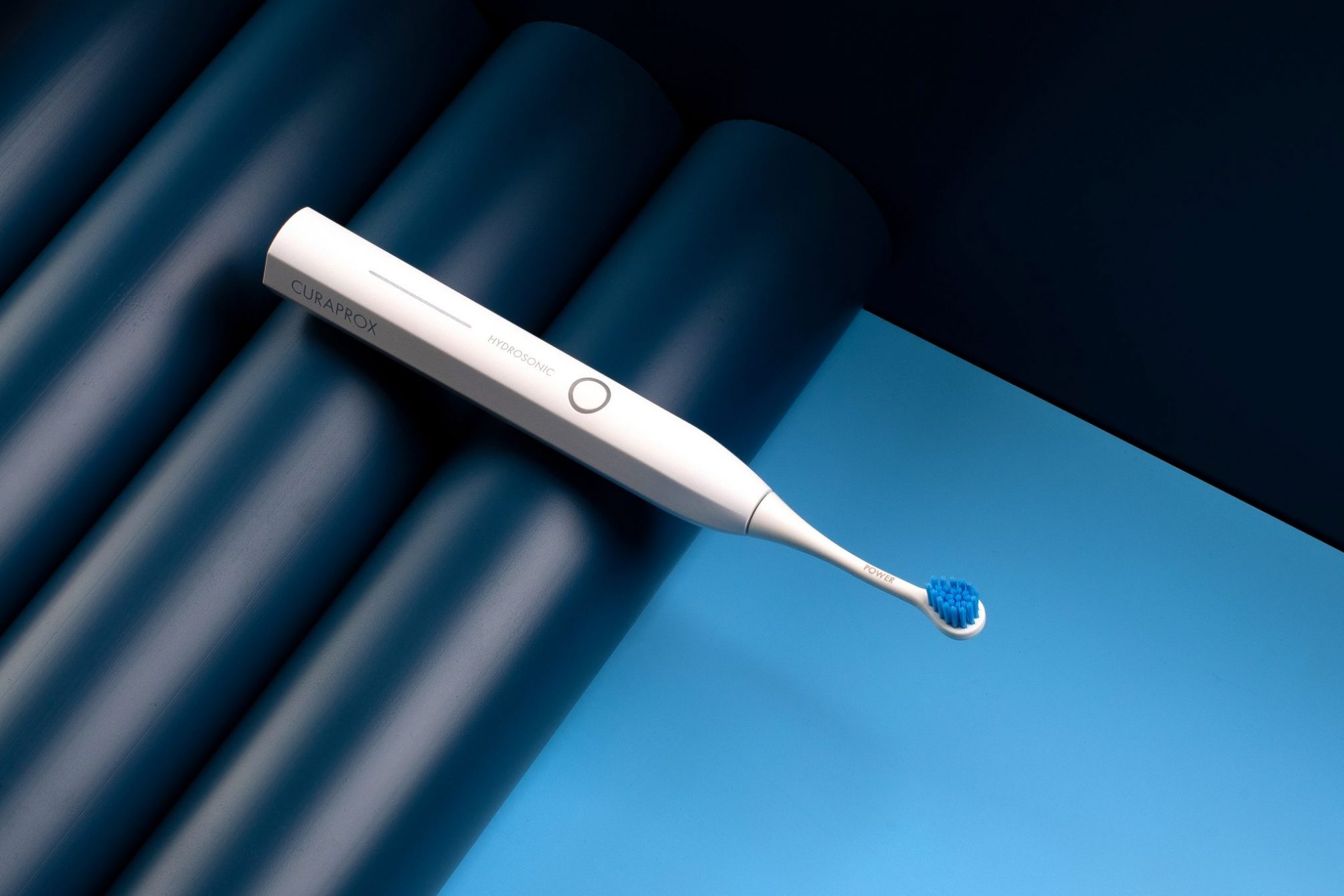
Fixed orthodontic devices make it easier for plaque to accumulate, and they make plaque removal harder. Currently, there is enough evidence of the efficacy of sonic toothbrushes and their superiority to manual brushing. Sonic brushes are especially effective, yet atraumatic and gentle on teeth and gingivae. A small, manoeuvrable brush head is important to remove plaque from in between brackets.